Define Antigen in Blood
When it comes to blood and immunity, one of the most important concepts to grasp is antigens. These tiny molecules play a crucial role in how our body identifies what belongs to us and what doesn’t. In the context of blood, antigens help determine blood types and can also influence medical procedures such as transfusions and organ transplants.
What is an Antigen?
An antigen is any substance that can trigger an immune response in the body. In simple terms, it is a marker or a “flag” present on the surface of cells, bacteria, viruses, or other foreign particles. The immune system recognizes these markers and decides whether the substance is safe or harmful.
When it comes to blood, antigens are proteins or sugars located on the surface of red blood cells (RBCs). These specific antigens are what define a person’s blood group.
Types of Antigens in Blood
The surface of human red blood cells carries hundreds of antigens, but only a few of them have major medical importance. These antigens are responsible for blood group classification and play a key role in safe transfusion and transplantation. The most important antigen systems are the ABO system, the Rh system, and a few other lesser-known but clinically significant groups.
1. ABO Antigens
The ABO blood group system is the most widely known and clinically significant. It was discovered by Karl Landsteiner in 1901, and it remains the cornerstone of transfusion medicine.
- A Antigen: People with blood type A have A antigens on their red blood cells. Their plasma naturally contains anti-B antibodies.
- B Antigen: People with blood type B have B antigens on their red blood cells, and their plasma contains anti-A antibodies.
- AB Antigen: People with blood type AB have both A and B antigens on their red blood cells. They do not produce anti-A or anti-B antibodies, making them universal recipients.
- O Type: People with blood type O have no A or B antigens on their red blood cells, but they produce both anti-A and anti-B antibodies. They are considered universal donors in emergencies, especially when Rh-negative.
The ABO system is critical because mismatches can lead to severe transfusion reactions.
2. Rh Antigens
The Rhesus (Rh) system is the second most important after ABO. It contains over 50 different antigens, but the most significant is the D antigen.
- Rh-Positive (Rh⁺): If a person has the D antigen, they are Rh-positive. About 85% of people worldwide fall into this group.
- Rh-Negative (Rh⁻): If a person lacks the D antigen, they are Rh-negative. This group is less common but medically important, especially during pregnancy and transfusion.
The Rh factor is vital in preventing hemolytic disease of the newborn (HDN) and ensuring safe transfusion. An Rh-negative individual should not receive Rh-positive blood, as their immune system may develop antibodies against it.
3. Kell Antigens
The Kell system includes several antigens, with the K (Kell) antigen being the most clinically significant.
It is found on the surface of red blood cells. Mismatched Kell antigens can cause hemolytic transfusion reactions and hemolytic disease of the newborn.
Though less common than ABO or Rh, Kell antigens are routinely checked in blood banks.
4. MNS Antigens
The MNS system includes M, N, S, and s antigens. These antigens are proteins located on the surface of red blood cells.
While not as dangerous as ABO or Rh mismatches, they can sometimes cause transfusion reactions.
MNS typing may be important in special transfusion cases or organ transplantation.
5. Duffy and Kidd Antigens
Other antigen systems, such as Duffy and Kidd, are also significant in transfusion medicine:
- Duffy Antigens (Fyᵃ, Fyᵇ): These are proteins that can act as receptors for certain malaria parasites (Plasmodium vivax). People who lack Duffy antigens may have natural resistance to this type of malaria.
- Kidd Antigens (Jkᵃ, Jkᵇ): These can sometimes cause delayed hemolytic transfusion reactions because the antibodies may not be immediately detectable.
6. Other Minor Antigen Systems
Besides the major systems mentioned above, there are more than 30 recognized blood group systems (such as Lutheran, Diego, and Lewis). While not all are routinely tested, they may still play a role in rare transfusion reactions or in specific populations.
In summary, ABO and Rh are the most critical for safe transfusions and pregnancy care. Kell, MNS, Duffy, and Kidd are clinically important in special cases. Other minor antigens may not always be tested but can still cause complications in rare situations.
Role of Antigens in Blood Transfusions
Blood transfusions are life-saving procedures, but they must be carried out with precision. The compatibility between donor and recipient blood is primarily determined by the antigens present on red blood cells.
If mismatched blood is given, the recipient’s immune system may recognize the donor’s antigens as foreign and launch a potentially fatal reaction.
Why Antigens Matter in Transfusions
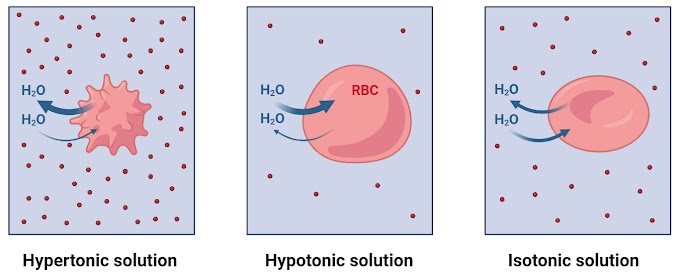
Self vs. Non-Self Recognition: The immune system uses antigens to distinguish the body’s own cells from invaders. When transfused blood carries antigens that the recipient’s body does not have, the immune system sees them as “foreign.”
Antibody Response: The body produces antibodies against foreign antigens. These antibodies bind to the mismatched red blood cells, causing them to clump together (agglutination) and eventually break apart (hemolysis).
Life-Threatening Reactions: This immune response can block blood vessels, damage organs, and cause severe complications such as kidney failure or shock.
Compatibility in the ABO System
The ABO system is the most critical in transfusion safety:
- Type A: Has A antigens → cannot receive B or AB blood (since it would introduce B antigens).
- Type B: Has B antigens → cannot receive A or AB blood.
- Type AB: Has both A and B antigens → can receive from all blood groups (universal recipient).
- Type O: Has no A or B antigens → can donate to all groups (universal donor), but can only receive type O blood.
Even a small amount of mismatched ABO blood can trigger a dangerous transfusion reaction.
Compatibility in the Rh System
The Rh factor is another crucial determinant in transfusion:
- Rh-Positive (Rh⁺): Can safely receive both Rh⁺ and Rh⁻ blood of the same ABO type.
- Rh-Negative (Rh⁻): Can only safely receive Rh⁻ blood. If given Rh⁺ blood, the immune system may form anti-D antibodies.
Once anti-D antibodies develop, any future exposure to Rh⁺ blood can cause severe transfusion reactions or pregnancy complications.
Universal Donors and Recipients
- O Negative (O⁻): Known as the universal donor because it lacks A, B, and Rh antigens. It is often used in emergencies when the recipient’s blood type is unknown.
- AB Positive (AB⁺): Known as the universal recipient because these individuals have all major antigens and thus do not form antibodies against A, B, or Rh.
Consequences of Antigen Mismatch
If the donor and recipient blood are incompatible, the following can occur:
- Acute Hemolytic Reaction: Immediate destruction of transfused red blood cells, leading to fever, chills, chest pain, low blood pressure, and organ damage.
- Delayed Hemolytic Reaction: Occurs days to weeks later, often due to antibodies against minor antigens (e.g., Kidd, Duffy). Symptoms may be mild but can still reduce transfusion effectiveness.
- Alloimmunization: Repeated transfusions can lead to the development of antibodies against multiple antigens, making it harder to find compatible blood in the future.
Cross-Matching: Ensuring Safety
To prevent these complications, blood banks perform compatibility testing before transfusion:
- ABO and Rh Typing: Determines the patient’s blood group.
- Antibody Screening: Detects unexpected antibodies in the patient’s plasma.
- Cross-Matching: Mixes donor blood with recipient plasma in the lab to ensure no reaction occurs.
This multi-step process helps ensure that the transfusion will be safe and effective. In short, antigens are the “identity tags” of red blood cells, and matching them correctly during transfusions can be the difference between saving a life and causing a dangerous reaction.
Antigens in Pregnancy
During pregnancy, the relationship between the mother’s and the baby’s blood can be influenced by antigens, especially those of the Rh system.
While the mother and baby do not normally share blood directly, small amounts of fetal blood can enter the mother’s circulation.
If the baby’s blood contains antigens that the mother’s immune system does not recognize, complications can arise.
Role of Rh Factor
The Rh factor is the most clinically significant antigen in pregnancy:
Rh-Positive Baby, Rh-Negative Mother: If the baby inherits the Rh (D) antigen from the father, and the mother lacks it (Rh⁻), her immune system may see the baby’s red blood cells as “foreign.”
Antibody Production: The mother’s immune system can produce anti-D antibodies against the baby’s red blood cells.
First Pregnancy vs. Future Pregnancies: In the first pregnancy, the risk is usually low because antibody production is often slow and limited.
In subsequent pregnancies, if the baby is again Rh⁺, the mother’s immune system responds much more quickly, attacking the baby’s red blood cells.
Hemolytic Disease of the Newborn (HDN)
If maternal antibodies cross the placenta and attack the fetal red blood cells, it leads to a condition called Hemolytic Disease of the Newborn (HDN), also known as erythroblastosis fetalis.
Fetal red blood cells are destroyed (hemolysis). This causes anemia, which may result in poor oxygen delivery to the baby’s organs. In severe cases, the baby may develop jaundice, heart failure, or even death before or shortly after birth.
Prevention of Rh Incompatibility: Modern medicine has made HDN largely preventable through Rh Immunoglobulin (RhIg or Rho(D) immune globulin). It is given to Rh-negative mothers during pregnancy (around 28 weeks) and again after delivery if the baby is Rh-positive.
This injection prevents the mother’s immune system from developing anti-D antibodies by “neutralizing” fetal Rh-positive cells before her body reacts.
Testing and Monitoring: Pregnant women undergo blood typing and antibody screening early in pregnancy.
If antibodies are detected, doctors monitor the baby closely with ultrasounds and sometimes blood tests to check for anemia.
Conclusion
Antigens in blood are not just biological markers; they are essential in defining blood types, ensuring safe transfusions, and protecting pregnancies. From the ABO and Rh systems to other lesser-known antigens like Kell, Kidd, and Duffy, these tiny molecules have a powerful influence on medical practice.
Whether preventing life-threatening transfusion reactions or managing complications in pregnancy, understanding antigens has transformed modern healthcare. In short, knowing how antigens work saves lives every single day.
Some Short Questions and Answers
1. What are blood antigens?
A. Blood antigens are proteins or sugars found on the surface of red blood cells that determine blood type and trigger immune responses.
2. Why are antigens important in blood transfusions?
A. They ensure compatibility between donor and recipient blood. A mismatch can cause dangerous immune reactions.
3. What is the difference between Rh-positive and Rh-negative?
A. Rh-positive blood has the D antigen, while Rh-negative blood lacks it. This factor is crucial in transfusions and pregnancy care.
4. Can antigens affect pregnancy?
A. Yes. If an Rh-negative mother carries an Rh-positive baby, her immune system may attack the baby’s red blood cells, causing Hemolytic Disease of the Newborn (HDN).
5. Which blood type is considered the universal donor?
A. O negative (O⁻) is the universal donor because it lacks A, B, and Rh antigens, minimizing the risk of immune reactions.




0 Comments